With an Urgent Need, Researchers Develop Multi-Patient Ventilators

Shuttered labs and social distancing haven’t gotten in the way of two research teams’ efforts to create a ventilator capable of treating multiple patients.
Everyone knows about the shortage of ventilators across the globe, and the difficulty in getting companies to begin producing enough of them at scale to ensure everyone who needs one has access to the lifesaving equipment. One solution—multiplication—has been to hasten the manufacturing process. Another solution, preferred by entrepreneurs like Elon Musk, is to retrofit other devices to provide the same service.
Two research teams at Yale are trying something different. The lab of Laura Niklason, MD, PhD, and the Coalition for Health Innovation in Medical Emergencies (CHIME), a multidisciplinary group that came together in March to address innovations related to COVID-19, are developing ways to allow a ventilator to treat multiple patients at a time.
Niklason, the Nicholas M. Greene Professor at Yale University in Anesthesia and Biomedical Engineering, became involved in the effort after an informal group dedicated to researching ventilator splitters reached out to her. With her lab closed to abide by social distancing restrictions, and a background in pulmonary architecture (Niklason focuses on growing lungs from scratch), Niklason mobilized her team to look at what could be done.
“A lot of companies were volunteering to build ventilators, and that’s the safest way to go, one ventilator per patient, so building more of those was our first impulse,” said Sam Brickman Raredon, a member of the Niklason lab in Yale School of Medicine’s MD-PhD program. “But reengineering and approving a ventilator from scratch is really difficult and time-consuming. We needed another, more accessible solution.”

Drawing on examples of crises where ventilators had been in short supply, Niklason’s team realized that another way to provide treatment might be to use ventilators for more than one patient at a time—to divide them for use among multiple patients. Of particular interest was a paper co-authored by Charlene Babcock, MD, and Greg Nyman, MD, which had been published in 2006 about the possibility of using ventilators to treat up to four patients simultaneously.
According to Clark Fisher, MD, PhD, a resident in the department of anesthesiology who had worked with Niklason in the past, Babcock and Nyman’s hypothetical procedure was put into practice at least once, out of desperation, during the Las Vegas shooting of 2017. There, local hospitals had been briefly overwhelmed by patients from the mass casualty event. The article hadn’t been reviewed comprehensively since.
Digging into the paper, the results of Las Vegas, and efforts to replicate Las Vegas in hospital ICUs in Italy and the United States, Niklason’s team identified a problem. In Las Vegas, concert-goers had mostly been young, healthy people without underlying conditions. The improvised ventilator splitters were employed for hours, no more than a day at a time, for people in otherwise good shape, who happened to have been shot. This meant that patients of similar size and health could be intubated simultaneously, and briefly, as an immediate lifesaving measure.
“Intubating someone with a healthy pair of lungs, even one that has been injured through trauma, is very different from what we’re seeing with COVID-19,” Fisher said.
Patients of COVID-19 require ventilators for much longer, and have wildly varying physiological and immunological profiles. This means simply dividing a ventilator’s capacity between two patients isn’t sufficient—a setting that stabilizes one patient could make another patient far worse. In a life-and-death situation, hospitals across the world had been employing Babcock and Nyman’s hypothesis, wagering that a chance at life was better than no chance at all.
Niklason’s team hit upon a more nuanced system, which they named “PReVentS,” or the Pressure Regulated Ventilator Splitting response paradigm. It depends on the fact that patients require ventilators to supply their lungs with oxygen by volume, or by pressure—and COVID-19 patients are very sensitive to volume, which can cause irreparable damage to lung tissue over time. It isn’t difficult to “split” a ventilator to pump air into a patient’s lungs by volume. Pressure—something that up until now could only be delivered by individual ventilators—is key to ensuring that COVID-19 patients receive the best treatment possible.
“As far as I know, we have the only device that allows a single ventilator to simultaneously treat two totally different patient profiles,” said Niklason.
“If two patients have the same profile, then a ventilator splitter is probably sufficient; that requires a lot of analysis on the part of doctors,” said Fisher. “And from what I hear, there isn’t a ton of time in the ICUs at the moment.”
The CHIME team, which operates out of the Center for Engineering Innovation & Design (CEID), has been working with various groups at the School of Medicine, including the Niklason lab.
“They know the best way to do this from a clinical patient perspective and told us what they need from an engineering perspective,” said Joe Belter, who’s leading CHIME’s ventilator efforts. “The people in Niklason’s group came up with some really clever ways of routing air to two different patients using some off-the shelf components, and the CHIME group has been assisting, trying to make that assembly a little more user-friendly.”
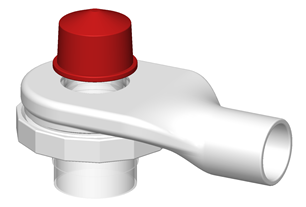
Essentially, he said, they want to develop a design that easy for hospital staff to put together and use in a very high-stress environment. After creating some computer-aided designs, the team printed out prototypes at the CEID, the Wright Laboratory, the School of Architecture, and even Belter’s home office. Those were then handed over to the Niklason group so they could review it and work through some of the layouts.
PReVentS is a device that allows one ventilator to treat two patients simultaneously, and, critically, individually—functionally dividing the ventilator into two. While the PReVentS splitter is designed for simultaneous use by two patients, according to Raredon, Babcock’s paper establishes that it should be possible to use a single ventilator for up to four patients.
From its inception as an idea at the end of March, it took about two weeks of working with engineers, clinicians, and other specialist consultants to develop the prototype, a video of which was posted to Twitter on Tuesday, April 7th (see below).
Before sharing the video, the team shared a preprint of their work on MedRxiv an open-source repository shared by Yale, the British Medical Journal, and the Cold Spring Harbor Laboratory. The goal is to share this work with other teams working along similar lines, to accelerate the procurement of effective quality ventilator splitters in ICUs before they are overwhelmed by ventilator need.
“Every piece of the device is from parts that one can find on the shelf of your local hardware store,” said Raredon. He also believes that it will be simple to 3D print those pieces that aren’t available.
This is an advantage in more ways than one, according to Niklason; “it’s a lot easier to stockpile tubing than additional ventilators,” she said.
Niklason and her team are motivated to finish work on PReVentS. “There’s a tremendous feeling of urgency and immediacy,” said Niklason. “Our lab has operated at the intersection of lung medicine and bioengineering for a long time—we were a natural to work on the problem. Now it’s a matter of finishing it; not just for this illness, but for any future similar illness, too.”
A Different Kind of Timeline
Unlike a lot of work in academia, the efforts of Niklason’s lab and CHIME are moving at an incredibly fast pace.
“We’re trying to address an immediate response - that is, what can we do in the next two weeks to address this?” said CHIME member Joe Belter, who’s leading the ventilator project. Ideally, he said, there would be enough time to take existing ventilator designs and make more of them. But that’s not the case. “There’s a gap in need between when those are available and now, and there are already hospitals that have expressed a need for ventilators - so, yes, it’s a very fast timeline.”
In addition to working with the Niklason lab, CHIME has been exploring other ways to design a device that can be 3D-printed, added to a standard ventilator, and allow for the ventilation of multiple patients while still independently controlling the air flow to each. When putting together some prototypes, a major part of the process involved consulting with Yale alumna Becky Robinson-Zeigler, PhD. The Deputy Chief Regulatory Officer with the Advanced Regenerative Manufacturing Institute with nearly seven years of experience at the U.S. Food & Drug Administration (FDA), Robinson-Zeigler advised the team on certifications and tests that pertain to this work.
Belter welcomes the additional scrutiny, as it helps ensure that the product will be safe and reliable. It also helps that the FDA has eased up certain regulations to facilitate innovations that are critical during the COVID-19 crisis.
“They’ve been very supportive of efforts to put new ventilators out there and to proposals for new techniques for splitting ventilation between patients,” he said.
Belter, a Yale alumnus, is director of actuator engineering with ClearMotion, which builds software-enabled vehicle suspension systems. He said there’s a fair amount of overlap between his day job and his work with CHIME. “Hydraulic systems are all about flows and pressures, and the same principles apply to ventilators.”
In addition to Belter and Robinson-Zeigler, the team includes particle physicist and associate director for instrumentation and education James Nikkel, PhD, and Dr. Daniel Wiznia, assistant professor of orthopaedic surgery. Joe Zinter, PhD, assistant director of the CEID, said the team was designed to have a diverse set of backgrounds - something that the ambitious project required.
“We wanted a multidisciplinary team that could look at these problems from new and different perspectives,” said Zinter, who is helping to coordinate CHIME’s efforts.
Like Niklason’s team, CHIME members are aiming for a device that accommodates the differences in individual patients, such as lung capacity.
“We want something that allows for each patient to have a more controlled ventilation set of parameters, and allows for some level of independence of the two patients beyond what you would have with a Y-splitter between two patients,” Belter said.
The next step, he said, is working with local companies to manufacture them in a quality-controlled environment that meets ISO-certification standards. “We’re sending them the files and they’ll be able to print those for us in a more controlled environment, using a biocompatible material.”
Naftali Kaminski, chief of pulmonary, critical care, and sleep medicine at Yale School of Medicine, said the progress made by Niklason’s lab and CHIME in such a short time has been tremendous.
“These two initiatives are amazing,” he said. “They have different names, but I think they should both be the Yale Ventilator Solutions.”

