To Relieve a Critical Shortage, a Way to Test Face Masks

With certified face masks at a critical shortage, a team of researchers at the School of Engineering & Applied Science are developing a system to test the reliability of non-standard face masks.
 Face masks typically worn by healthcare workers undergo tests to ensure that they adequately protect users. The most commonly used among them are known as N95 masks (so called because they filter out at least 95% of fine airborne particles), which have been certified by the National Institute for Occupational Safety and Health (NIOSH). However, a severe shortage of these tested masks means healthcare workers may have to rely on masks that have not been tested by the same methods - many of which are arriving at hospitals in need, including Yale-New Haven Hospital.
Face masks typically worn by healthcare workers undergo tests to ensure that they adequately protect users. The most commonly used among them are known as N95 masks (so called because they filter out at least 95% of fine airborne particles), which have been certified by the National Institute for Occupational Safety and Health (NIOSH). However, a severe shortage of these tested masks means healthcare workers may have to rely on masks that have not been tested by the same methods - many of which are arriving at hospitals in need, including Yale-New Haven Hospital.
“Some of the masks that have come in have been internationally sourced and don't have a NIOSH certification,” said SEAS Deputy Dean Vincent Wilczynski.
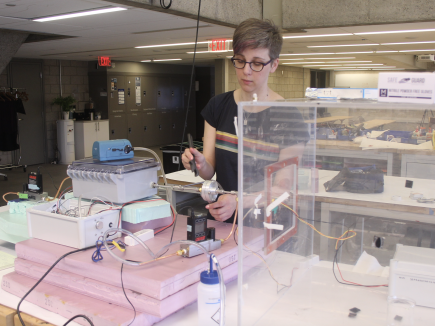
The team, led jointly by Lawrence Wilen, senior research scientist at the Center for Engineering Innovation & Design (CEID), and associate research scientist Kate Schilling, is designing a system that would give healthcare workers informed choices about how well these masks work.
“Currently, we don’t know what their capabilities are in terms of preventing coronavirus transmission,” Schilling said. “That’s a big problem, so what we’re looking at are two specific questions. The first is flow impedance: Can you actually breathe through these masks? The second question is particle transmission or filtration – are the masks actually removing these particles?” Specifically, she said, the test measures a range of particles from small droplet nuclei to larger respiratory droplets, both of which the World Health Organization is looking at in evaluating coronavirus transmission.
The results can then be compared to those of the NIOSH-certified masks and the test data will be relayed to environmental safety and medical professionals for their assessment.”
Wilen and Schilling have been building the system in the John Klingenstein '50 Design Lab at the CEID. To do so, they’ve borrowed equipment from the labs of Juan de la Mora, professor of mechanical engineering & materials science, Drew Gentner, associate professor of chemical & environmental engineering, and Krystal Pollitt, assistant professor of epidemiology and chemical & environmental engineering.
“If we can use this setup to test those batches of masks as they come in, it means that we can screen out the masks that are poorly performing,” Gentner said.
The device relies on a a stick of smoldering incense in a one-cubic-meter box that creates a stable aerosol population with particles of various sizes. The researchers can then examine a wide range of particle sizes – from the size of those similar to what would be found in human-related aerosols generated by coughing, sneezing, talking, and exhaling, all the way down to tiny droplets the WHO call “droplet nuclei.”

“The experimental setup allows the team to monitor changes in that distribution of aerosols so we can specifically examine the size-dependent particle concentrations that pass through the filter,” Gentner said. “We have a system of mass flow controllers where we can control the flow rate, so we can mimic the different rates across a single breath that a human might have depending on their activity.”
Understanding how breathable a mask is, Wilen said, is a critical part of the assessment.
“You want it to seal to your face, but still allow you to be able to breathe and provide enough flow without having to use too much pressure,” he said. To that end, a separate device pushes air through a filter and measures the flow impedance.
Wilczynski noted that the matter requires a collaboration of a wide range of knowledge and resources. In addition to the project being headed up by Wilen, who has a Ph.D. in physics, and Schilling, whose Ph.D. is in chemistry, it’s also using equipment and expertise from the departments of chemical & environmental engineering, and mechanical engineering.
“They’re all using their backgrounds in each discipline to take on the issue of mask testing,” he said.
It also requires that they do this work very quickly. Rather than working on a problem over a long period, as is often the case in academia, the researchers have only days. That means a lot of learning things on the fly and rapid design iterations. Without the immediate use of an atomizer to generate an aerosol, they used incense instead, which in some ways suits their purposes better. Another example of quick work is in the Machine Shop in the basement of Dunham Laboratory, where Research Support Specialist Nicholas Bernardo where he “scrounged up some materials” to fashion from scratch a new filter holder made out of aluminum for the device (existing models are made out of Teflon, which wouldn’t work for this device). He made the first component in six hours.
The outbreak is a new problem, Gentner said, but much of the science behind it overlaps with many fields of research at the university.
“COVID-19 is a completely new issue that we haven't worked on before, but in many ways, it returns to aerosol science and we’ve all spent a lot of time thinking about aerosols - so going back to those fundamentals is really helpful.”
This project is one component of a number of activities organized by the Coalition for Health Innovations in Medical Emergencies (CHIME), a team of Yale domain experts and practitioners in the fields of public health, nursing, emergency medicine, design, engineering, and communications who are addressing immediate needs regarding the shortage of PPE and other medical technologies needed for COVID-19 medical care.

