Students Present Medical Innovations

The student teams of Medical Device Design and Innovation (MENG/BENG 404) recently presented their medical innovations. Co-taught by Dr. Daniel Wiznia, assistant professor of orthopedics and rehabilitation and mechanical engineering and materials science, and Steve Tommasini, research scientist at the School of Medicine, the course brings together interdisciplinary teams of students with physicians from the Yale School of Medicine and Yale-New Haven Hospital to address unmet clinical needs.
The teams presented their projects, which were initiated at the Center for Engineering Innovation & Design (CEID) and completed virtually, last week:
A more reliable hip replacement
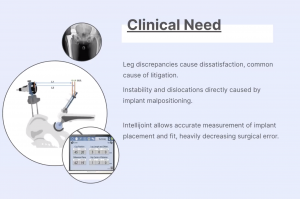 About 400,000 total hip replacement surgeries are performed annually. The team of Anusha Manglik ‘21, graduate student Yanning Liu, Tom Postiglione ‘21, and Oyinda Alliyu, 20 worked to improve on one aspect of Intellijoint, a surgeon-controlled navigation system. It allows the accurate measurement of implant placement and fit, heavily decreasing surgical error. However, dislocation of its platform can lead to inaccurate measurements or inability to capture measurements.
About 400,000 total hip replacement surgeries are performed annually. The team of Anusha Manglik ‘21, graduate student Yanning Liu, Tom Postiglione ‘21, and Oyinda Alliyu, 20 worked to improve on one aspect of Intellijoint, a surgeon-controlled navigation system. It allows the accurate measurement of implant placement and fit, heavily decreasing surgical error. However, dislocation of its platform can lead to inaccurate measurements or inability to capture measurements.
The student team developed a system that modifies the femur platform on the Intellijoint HIP navigation tool to be more stable. Inspired by the drywall bolt used for home applications, they created a device designed to attach the platform to the bone. In addition to 3D prints from the CEID, the home-bound team members used household materials to prototype the device, including super glue, aluminum foil, plastic straws, and sheet metal.
A quieter biopsy
More than 1 million prostate biopsies are performed annually, and the standard method can be stressful and painful. The team of Max Bottene ‘20, Lena Goldstein ‘22, Nguyen Pham ‘21, Cedrick Lingane ‘20 focused on one aspect of the biopsy gun used to diagnose prostate cancer - specifically how noisy it is: volumes can reach about 107 decibels.
They built a prototype of a biopsy gun with two chambers with acoustic dampening material. By doing so, they were able to reduce the volume to about 58 decibels - about the same as the loading mechanism of the gun. Due to limitations of the second chamber, though, they redesigned the schematic to eliminate the second chamber and instead create a larger single chamber that holds more acoustic dampening material.
 A better way to fix small bones
A better way to fix small bones
Foot injuries caused by high-impact collision present a challenge to surgeons. The team of Shelby Meckstroth ‘20, Stephanie Blas-Lizarazo ‘20, Trevor Chan ‘20, Ivan Lima-Bravo ‘20, Kyle Almquist ‘20, Nick Szabo ‘20 set out to make treatment easier and more reliable.
To treat injuries to areas of small bones, the bones need to be separated, cleaned of cartilage and residue, set, and clamped so they can fuse together. Current devices, though, aren’t perfect and can lead to an unequal force distribution throughout the fracture. This can make it difficult to clean the entire bone surface, and can leave space at the far end for scar tissue to form, which can lead to a weaker bone.
The students made a foot and ankle retractor that gives surgeons better access to the bone surfaces, and clamps them together so the surfaces are flush and don’t leave small pockets where scar tissue forms.
Simplifying Fracture Treatment
About 10% of all fractures in children occur at the proximal humerus, the bone that extends from the shoulder to the elbow. The team of Lauren Chapey ‘20, Nataly Moreno ‘21, Ting Gao ‘20, Vishal Patel ‘20, and graduate student Sam Cabot created a device aimed for children between ages 2 and 14 designed to improve the treatment of those injuries.
Immobilization is usually enough, but excessive shortening, angulation, or malrotation at the fracture site can require operative intervention. The standard current treatment involves Kirschner wires (or “k-wires): sterilized, sharpened, smooth stainless steel pins. It’s a well-established method, but not without complications. They have the potential to move deeper into the bone (known as “migration”), they can fracture, cause infection, and the wires can stick out as much as an inch outside the arm.
To prevent these complications, the students created a device that externally fastens k-wires to one another and limits their mobility. Additionally, the team is working on a motion sensor that warns the child if he or she is moving too much.
Helping nurses with technology
Only 51% of registered nurses surveyed said they have enough staff to handle the workload in their hospitals. To help optimize their workload, the team of Sinem Sinmaz ‘20, Ali Brocato ‘22, Ruochen Zhang ‘20, and Matt Spero ‘21, developed Advance: AI Driven Virtual Assistant Nursing Communication Enhancer.
Using voice-activated software, the system would allow direct communication between patients and nurses. Among other features, it would allow for estimated time arrivals (similar to those used with Uber) for patients to view on their televisions or repeated back to them on Alexa. Patients can also request updates or push to remind the proper caretaker of their request, and nurses automatically have requests arranged in their inbox by prioritization levels.

