Nanoparticles Deliver Treatment Directly to Tumors of Deadly Brain Cancer
Using nanoparticles administered directly into the cerebrospinal fluid (CSF), a research team has developed a treatment that may overcome significant challenges in treating a particularly deadly brain cancer.
 The researchers, led by professors Mark Saltzman and Ranjit Bindra, administered to mice with medulloblastoma a treatment that features specially designed drug-carrying nanoparticles. The study, published in Science Translational Medicine, showed that mice who received this treatment lived significantly longer than mice in the control group.
The researchers, led by professors Mark Saltzman and Ranjit Bindra, administered to mice with medulloblastoma a treatment that features specially designed drug-carrying nanoparticles. The study, published in Science Translational Medicine, showed that mice who received this treatment lived significantly longer than mice in the control group.
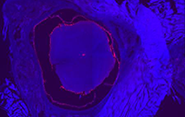
Medulloblastoma, a brain cancer that predominantly affects children, often begins with a tumor deep inside the brain. The cancer is prone to spread along two protective membranes known as the leptomeninges throughout the central nervous system, particularly the surface of the brain and the CSF. Leptomeningeal spread is seen in a number of primary brain tumors, as well as in brain metastases from solid tumors in the breast, lung, and other places. Because there are no anatomic barriers in the CSF to prevent further growth, these cancers can spread rapidly.
Targeting tumors in the CSF has proven difficult, in part because the fluid rapidly cycles through the central nervous system about four times a day in humans, typically flushing away anti-tumor drugs before they’ve had a chance to accumulate and have any effect.
“It's like a waterfall system, with a fast, rapid fluid flow,” said Minsoo Khang, lead author of the study and a former graduate student in Saltzman’s lab.
To get around this obstacle, the research team fabricated nanoparticles that adhere to tumors. Designed in Saltzman’s lab, these nanoparticles are made with degradable polymers that slowly release a DNA repair inhibitor, talazoparib, which is FDA-approved and currently used in the clinic for a number of cancers. The drug is one of a relatively new class of cancer drugs known as PARP inhibitors, which block an enzyme that helps repair DNA. Without the ability to repair their DNA, tumor cells are more likely to die.
The nanoparticle treatment is injected intrathecally - that is, it’s delivered directly between the leptomeninges protecting the CSF. Over a period of weeks, the researchers detected the presence of the nanoparticles in the CSF for as long as 21 days after a single dosing.
“We were very excited to have found a medium that has long-term retention in this fluid space, which is otherwise challenging,” Khang said.
Treating brain cancers in general is challenging since few treatments can penetrate the blood-brain barrier, a natural defense system that can block potentially helpful drugs. The research team’s method could offer a solution.
“There’s been very little work on intrathecal delivery of nanoparticles, so we’re very excited because it can allow us to go after leptomeningeal spread of disease from brain metastases,” said Bindra, the Harvey and Kate Cushing Professor of Therapeutic Radiology and Professor of Pathology. “This has really opened up an entirely new way to treat these patients, although much more work needs to be done.”
Using the nanoparticles to target the tumors allowed the researchers to use the drug talazoparib, which has proven to be effective in a number of solid tumors outside of the brain. Because the drug has limited to no penetration of the central nervous system, however, an orally delivered dose would have limited efficacy against tumors with leptomeningeal spread.
“By encapsulating it in a nanoparticle and directly injecting it into the CSF, we now get very high exposure in just that area,” said Saltzman, the Goizueta Foundation Professor of Biomedical Engineering, Chemical & Environmental Engineering & Physiology, and a member of Yale Cancer Center.
Delivering the drug intrathecally also avoids injecting it directly into the brain, a technique referred to as convection-enhanced delivery, a very challenging procedure that can be performed only a few times a year. Intrathecal injections, in contrast, are much less invasive and can be given without a hospital stay.
“This is huge for us, because now we can do multiple nanoparticle treatments over time,” Bindra said.
In addition to the nanoparticle injection, mice were also given an oral dose of a chemotherapy drug known as temozolomide.
“It's a new platform where we can give these oral chemotherapies that get across the blood-brain barrier and a targeted agent just in the central nervous system,” Bindra said. “In essence, this compartmentalization of combination therapy will enhance synergistic tumor cell killing while minimizing systemic toxicity.”
The mice that received the nanoparticle-based treatment lived significantly longer than the mice who received drug therapy that didn’t use nanoparticles, and even longer than the mice that received no treatment. Further, there was much less spreading of the cancer in the mice that received the drug-carrying nanoparticles.
The researchers said the next steps will be to validate the approach in larger animal models, eventually followed by human testing. The team is also planning to test the treatment method on other cancers, particularly those that tend to spread to the brain.
Saltzman noted that the work was an interdisciplinary effort that drew on the expertise of numerous specialists. Other authors of the paper are Ju Hyun Lee, Teresa Lee, Hee-Won Suh, Supum Lee, Alessandra Cavaliere, Amy Rushing, Luiz H. Geraldo, Erika Belitzky, Samantha Rossano, Henk M. de Feyter, Kwangsoo Shin, Anita Huttner, Martine F. Roussel, Jean-Leon Thomas, Richard E. Carson, and Bernadette Marquez-Nostra.

